Electrophysiology Services & Treatment
City skyline
Electrophysiology is the cardiology specialty dedicated to treating heart rhythm disorders. Extensive services and treatment options are available for the diagnoses and treatment of electrical signals, or the rhythms of your heart. Today, many arrhythmias can be completely cured through a minimally invasive procedure called cardiac ablation. Others are treated and controlled by medication, pacemakers, defibrillators and/or non-surgical procedures. At Eastlake, our electrophysiologist uses the most advanced technology to detect, diagnose and treat arrhythmias including:
- Pacemaker Implantation
- Defibrillator Implantation (ICDs)
- Ablation procedures
- Pacemaker/ICD Follow-up
PACEMAKER / DEFIBRILLATOR FOLLOW-UP CLINIC
The Pacemaker / Defibrillator Clinic at Eastlake provides a vital part of our patient services. The clinic is staffed by RNs and CVTs (Cardiovascular Technician) and is overseen by our electrophysiologist, Dr. Moore. The clinic provides our patients with high quality care using state-of -the-art computerized technology.
The clinic provides complete pacemaker and/or defibrillator analysis for patients with implanted cardiac devices. We have the ability to assess appropriate function, test generator and lead integrity, retrieve abnormal heart rhythm information, assess battery and determine when replacement is imminent. Programming changes that are deemed necessary can be done during the clinic visit. The follow up clinic also allows some patients to do in-home, remote monitoring. Only certain devices are capable of this option. This system gathers information from patient devices and sends the data through a secured web site allowing patients to do routine follow up or have special situations reviewed. This allows the experienced pacemaker staff to review the data and promptly communicate with your cardiologist and/or Electrophysiologist which minimizes office visits.
PACEMAKERS
A pacemaker is a small device that is implanted in the upper chest region for prevention of an abnormally slow heartbeat. A slow heartbeat can develop when the heart’s natural pacemaker slows down with age or when the heart’s natural electrical conducting fibers wear out. Patients requiring pacemaker implantation often complain of dizziness, lightheadedness, fatigue and/or fainting associated with a slow pulse.
A pacemaker system generally consists of a pulse generator, which houses the pacemaker battery and circuitry, and two pacemaker leads. The leads are inserted through the veins into the top and bottom chambers of the heart.
A typical pacemaker implantation is done under local anesthesia with light sedation and can be completed within in 60 minutes. Patients with pacemakers can enjoy active, normal lifestyles with minimal restrictions. Most electronic devices in the environment, including microwave ovens, have no effect on pacemakers.
City skyline
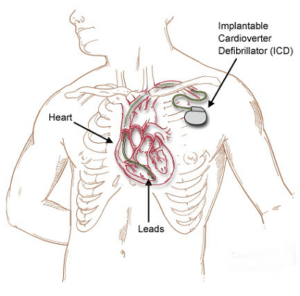
IMPLANTABLE CARDIOVERTER DEFIBRILLATOR
An implantable cardioverter defibrillator (ICD) is a small device that is placed in you chest. This device uses electrical pulses or shocks to help control life-threatening irregular heartbeats (arrhythmias); especially those that could lead the heart to suddenly stop beating (sudden cardiac arrest). When these arrhythmias occur, the heart can’t effectively pump blood, and a person will pass out within seconds and die within minutes if not treated. To prevent death, the condition must be treated right away with an electric shock to the heart. The treatment is called defibrillation.
An ICD has wire with electrodes on the ends that connect to the chambers of your heart. The ICD will continually monitor your heart rhythm. When the device detects that you are having an irregular rhythm, the ICD will use low-energy electrical pulses to restore a normal rhythm. If this doesn’t restore your normal heart rhythm, or if your ventricles start to quiver rather than contract strongly, the ICD will switch to high-energy pulses for defibrillation.
BIVENTRICULAR (BI-V) PACEMAKER
A Biventricular Pacemaker (Bi-V) is the newest type of pacemaker. It paces both sides of the heart simultaneously to coordinate their contractions and improve pumping ability. Some patients with moderate to severe heart failure also have a condition in which the two lower chambers of the heart are not beating at the same time. In normal hearts, both lower chambers (ventricles) beat together and are synchronized. When the ventricles are not beating in synchrony, heart failure symptoms may worsen. Bi-V pacemakers (also known as cardiac resynchronization therapy or CRT), along with medications, have been shown to improve patient’s quality of life and symptoms of heart failure.